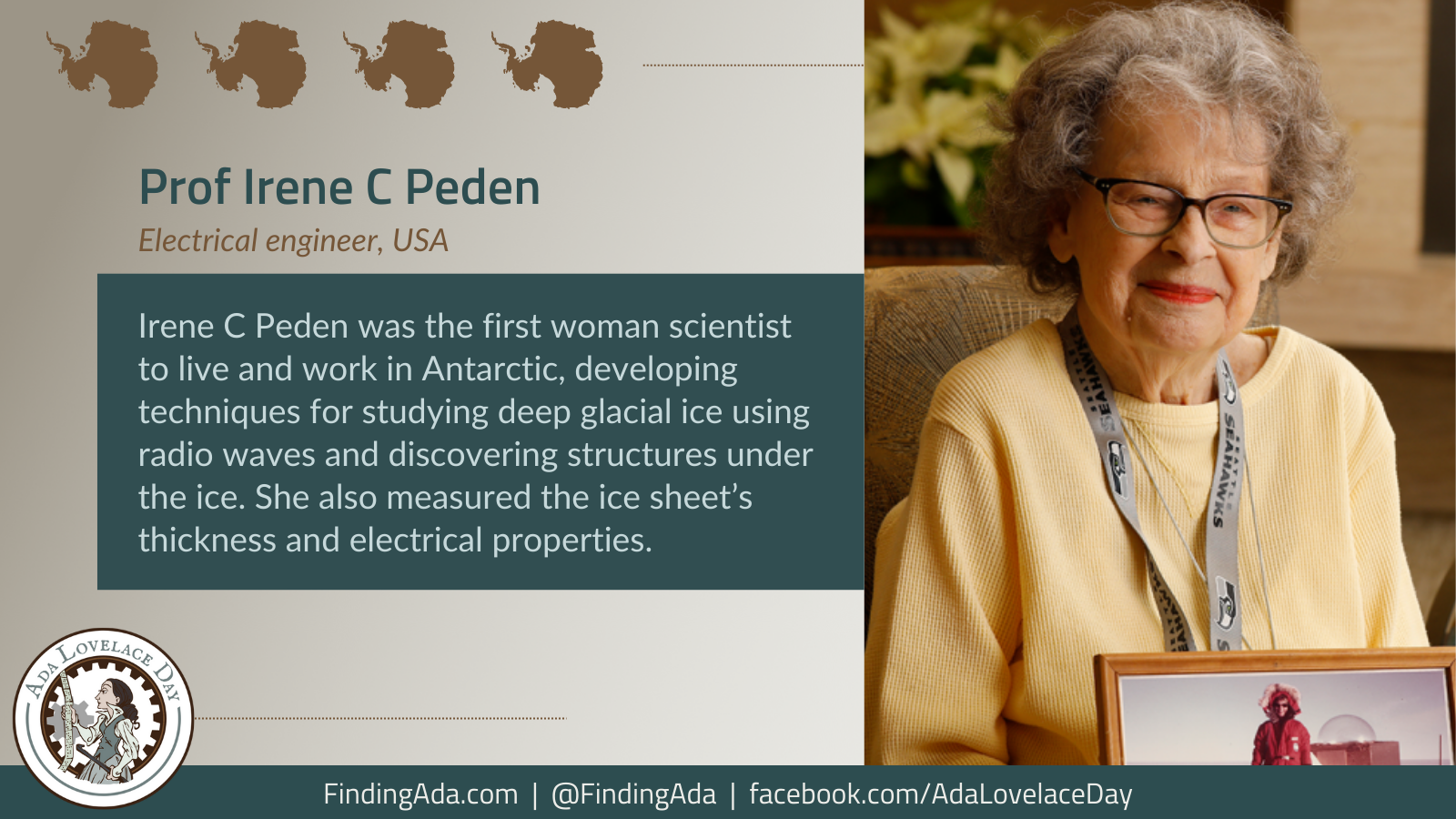
Professor Irene C Peden
Irene C Peden is an electrical engineer who was the first woman scientist to live and work in the interior of the Antarctic, developing techniques for studying deep glacial ice using radio waves.
Born in 1925 in Topeka, Kansas, Peden graduated from the University of Colorado when she was 22 with a degree in electrical engineering, although she was often the only woman in her classes. She worked in industry as an engineer from 1947 to 1954, but returned to education to get a masters and PhD from Stanford University, becoming the first woman to get a doctorate in electrical engineering from them. She joined the electrical engineering faculty at the University of Washington in 1961, again the first woman to do so. She served as president of the IEEE Antennas and Propagation Society, and was awarded their “Man of the Year” award. She was promoted to a professor in 1971, associate dean in 1973, and associate chair of the department in 1983.
She visited the Antarctic in 1970 to investigate the electrical characteristics of glacial ice, becoming the first female engineer or scientist to carry out research there. Because of the US Navy’s prohibition on women travelling alone to Antarctica, she had to find another woman to go with her but the New Zealand geophysicist who was supposed to join her failed her physical. Instead, a Christchurch librarian Julia Vickers, who was also an alpinist, took the job.
Three years earlier, the US Army Cold Regions Research Laboratories had drilled a 2.16km hole in the ice, and Pedersen lowered a probe 1.67km into the hole to study how very low frequency radio waves travelled through the ice. Her instruments also measured the electrical properties of the ice.
Because of the Navy’s scepticism of women, Peden was told that if she didn’t produce and publish robust scientific results, they would not allow other women to travel to Antarctica. Peden’s experiments were successful, and she expanded her work to measure the thickness of the ice sheets, and used very high frequency radio waves to discover structures under the ice. In 1979, she spent the whole winter at the South Pole, again the first woman to do so.
In 1993, she was named the National Science Foundation’s Engineer of the Year and was included in the American Society for Engineering Education’s Hall of Fame. A line of cliffs in Antarctica have been named after her by the Advisory Committee on Antarctic Names.
Further Reading
- Irene C. Peden, Wikipedia
- Antarctic trip was tip of the iceberg for this alumna, University of Colorado Boulder: CU Engineering Magazine 1 May 2018
- Professor Emerita Irene Peden receives Diamond Award, University of Washington: Electrical and Computer Engineering, 4 June 2018
- Trailblazing Engineer Irene Peden Broke Antarctic Barriers for Women, Kristen Pope, Smithsonian Magazine, 7 June 2019